
Infectious diseases have threatened the existence of mankind since ancient days. The Black Plague claimed more than 50 million lives in Europe in the 14th century and the sixth cholera pandemic took more than 800,000 lives between 1899-1923.
However, with the discovery of antimicrobials—thanks to Alexander Fleming’s accidental discovery of penicillin in 1928—we have been able to avert many infection-related deaths.
In the future, however, antimicrobials will be ineffective against infections—a phenomenon known as ‘antimicrobial resistance’—and will spell dire consequences for mankind.
What Is Antimicrobial Resistance (AMR)?
AMR is when microorganisms—bacteria, fungi, viruses and parasites—develop resistance against antimicrobial substances, such as antibiotics, rendering them ineffective.
While this is natural enough, unnecessary exploitation of antibiotics has expedited the process.
A groundbreaking 2019 report by the United Nations (UN) said ‘more and more common diseases, including respiratory and urinary tract infections, as well as sexually transmitted infections, are untreatable; lifesaving medical procedures are becoming much riskier, and our food systems are increasingly precarious.’
Currently, at least 700,000 deaths occur annually due to AMR. To put that in perspective: ischemic heart disease—or coronary heart disease—is the leading cause of death around the world with a global death toll of approximately nine million, but AMR could overtake this, if action is not taken, with the AMR death toll predicted to rise as high as 10 million per year, by 2050.
While a day when antimicrobials known to us will cease to work is inevitable, policymakers, healthcare workers, the general public and other stakeholders will play a huge role in determining how fast this day approaches.
In the meantime, alternate therapeutics such as phage therapy, probiotics and antimicrobial peptides are being investigated to be developed as the next weapon against infections.
How Bad Is The Situation In Sri Lanka?
“Sri Lanka is at a critical juncture in the fight against AMR,” Dr Shirani Chandrasiri, President of the Sri Lankan College of Microbiologists (SLCM) and member of the Antimicrobial Resistance Committee core group told Roar Media.
“South-East Asia is considered the hotspot of AMR, and the rates of AMR in Sri Lanka are alarmingly high. Of the urine infections I encounter weekly, at least 50 percent are resistant to first-line antibiotics. Deaths due to AMR are not an uncommon occurrence especially in the presence of other medical complications,” she said.
According to available AMR surveillance data from 2014, bacteria such as S.aureus (MRSA) and S. pneumoniae that cause life-threatening blood infections, pneumonia and meningitis have exhibited a resistance rate of 53 percent and 95 percent respectively, to first-line antibiotics. While Acinetobacter, a pathogen causing blood, urinary tract and lung infections showed a rate of 38 percent resistance to even the second-line antibiotics.
Several other studies have been carried out in Sri Lanka on knowledge of antibiotics among pharmacy students, the presence of resistant bacteria in patients at hospitals in Ragama, Maharagama, Peradeniya. Furthermore, the presence of resistant bacterial strains in Sri Lankan livestock, and even shrimp cultures are causes for concern, which evidently point out that AMR is something Sri Lanka needs to tackle swiftly.
National Steps Taken To Combat AMR
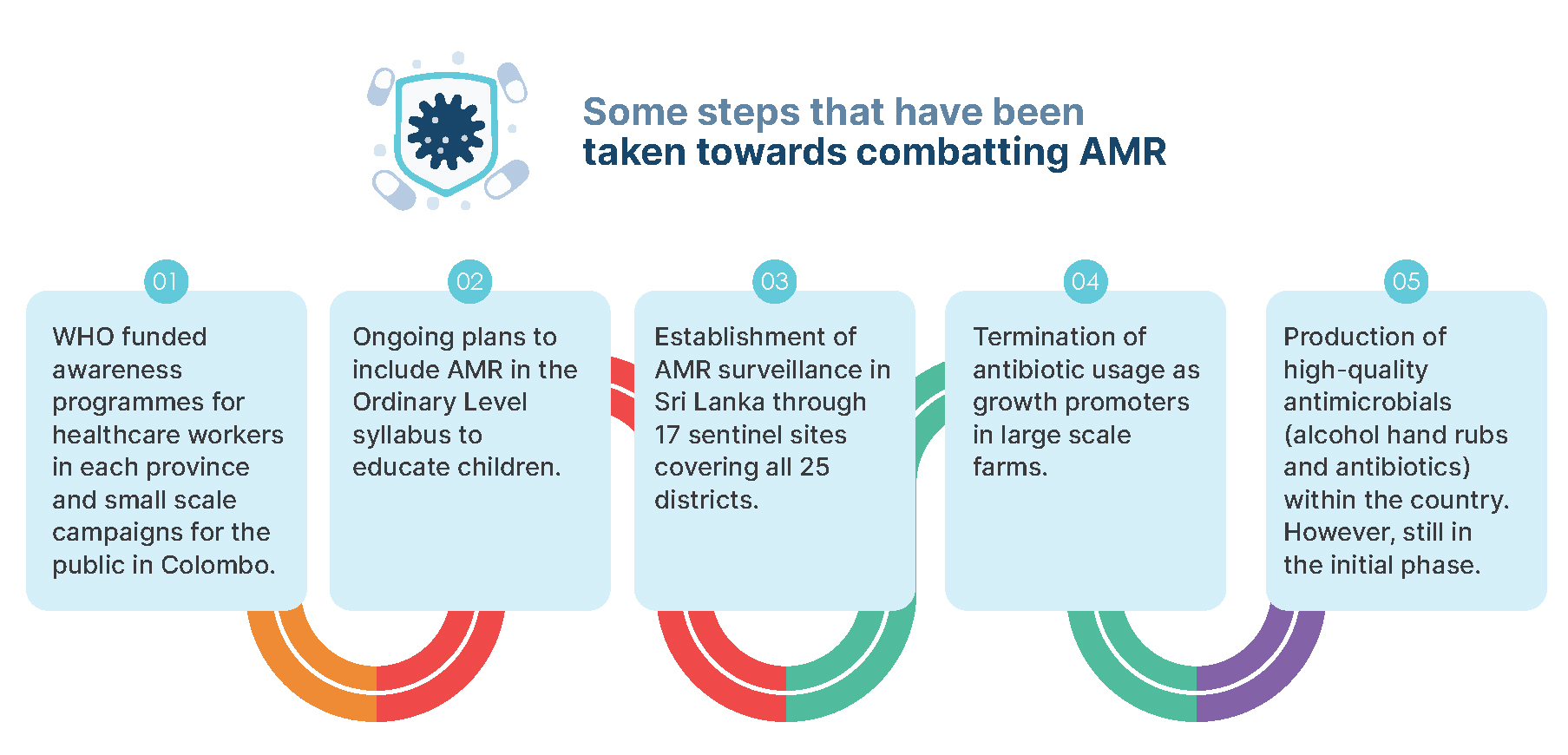
In 2016, the WHO-approved National Strategic Plan for Combatting Antimicrobial Resistance was implemented by Sri Lanka’s Ministry of Health and the SLCM. This Plan was to run from 2017-2022.

However, when inquired about the progress of the Plan, Dr Chandrasiri said, “unfortunately the progress of the Plan is further behind than expected due to various issues. While the government and WHO have been supportive, their patronage is needed in a bigger capacity for this plan to be carried out effectively.”
Funding is definitely a factor hindering the Plan, Dr Chandrasiri explained. She added that as Sri Lanka only has a handful of microbiologists within the country, it is difficult to launch out the Plan on a grand scale—this also since hospital consultations are quite demanding.
She also added that media coverage on the issue is much needed as this would be immensely helpful in creating awareness about AMR among the public. A national-scale awareness AMR campaign despite being in the planning, is yet to be carried out, the delay in this is mostly due to lack of funding and political support. Research to come up with novel diagnostics and vaccinations is scarce, which again, is due to a lack of funding within the country.
Why Is AMR Rising In Sri Lanka
There are quite a number of factors that drive AMR in Sri Lanka, including malpractices in the healthcare sector, such as inappropriate prescription of antibiotics by physicians, improper administration of antibiotics within inpatient care units or lack of antibiotic stewardship programs to educate the healthcare workers.
The use of antibiotics in food production, farms and agriculture are also steering causes of AMR. Misuse of antibiotics by people is another cause; for example, not completing a given course of antibiotics, self-prescribing antibiotics and using antibiotics prescribed for another person or illness. Further, the use of poor quality antimicrobials in Sri Lanka also exacerbates AMR.
Dr Chandrasiri weighed in on this and stated that even though laws are in place to prevent the availability of antimicrobials over the counter, these regulations are not strictly adhered to, especially outside of Colombo and its suburbs. She highlighted that monitoring the use of antibiotics by small-scale farmers is difficult, also due to the widely accepted notion that most small scale farmers use antibiotics as a preventative measure to safeguard livestock from infections, that are mostly caused by viruses. Dr Chandrasiri added that, “a lack of awareness among people is one of the biggest hurdles that promote AMR in Sri Lanka.”
What Can We, The General Public Do?
A great deal can be achieved if the general public worked towards combatting AMR. Dr Chandrasiri let us in on a few pointers that we can implement individually.
- Do not take antibiotics over the counter for any reason, this includes diarrhea, sore throats, colds and fevers. Since most of these illnesses are caused by viruses to which antibiotics are ineffective.
- When prescribed a course of antibiotics, complete the entire course even if you start feeling better before it ends.
- Do not share your prescription with a person who may have the same symptoms as you.
- Do not take antibiotics as a precautionary measure during a flu season without a doctor’s advice.
- If your doctor prescribes antibiotics based on your clinical symptoms, discuss the possibility of carrying out laboratory investigations before the prescriptions of antibiotics. While this may seem like a drastic measure, taking antibiotics unnecessarily can cripple your health too by disturbing your gut flora.
AMR is rarely seen as a threat to those outside the scientific community in Sri Lanka, despite AMR being one of the biggest health threats to the world. It would be best for each of us to act now before the situation boils over and threatens the health of our future generations. Therefore, each person implementing little steps will help curb AMR, at least until new alternatives to antibiotics are developed and made available for use.








